Borrelia has been around it seems forever and occurs on all continents from the tropics to the arctic circle.
Humans have had plenty of time to develop our defences against Borrelia. This probably explains why many people don’t become severely ill with an acute infection of the illness. As soon as Borrelia is injected into a person’s system, usually by tick bite, their immune system is activated and begins attacking and clearing the microbe.
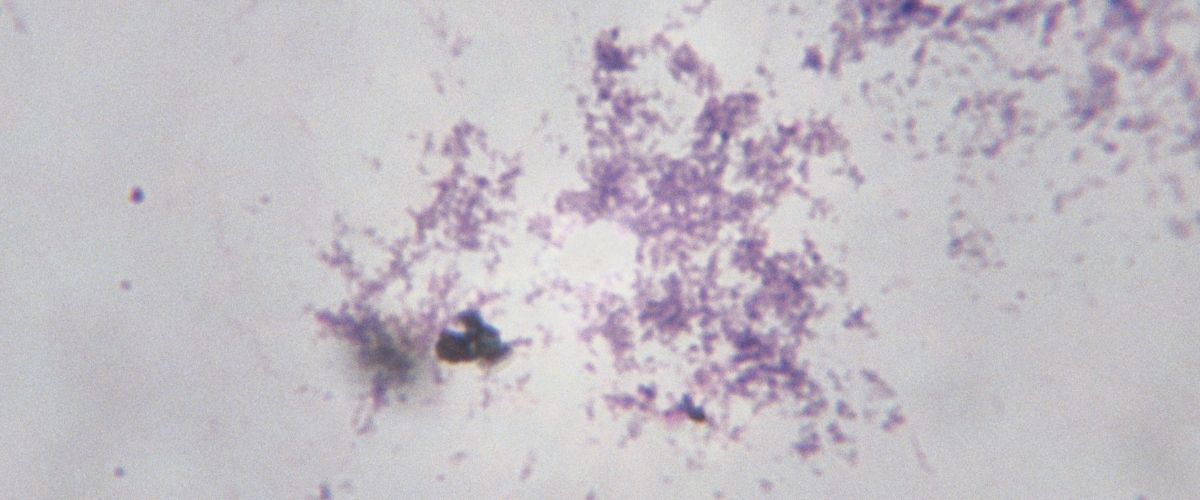
Borrelia, however, is a master at persisting in the body and the infection easily becomes chronic. How? Because it can live inside cells. As soon as the Borrelia microbes enter the body, they work at infecting the white blood cells (WBCs) of the immune system.
Borrelia’s ability to infect WBCs allows them to do two important things:
- Once inside WBCs, which are in your bloodstream, they can gain access to tissues throughout the body. Once in a new location, it is easy for them to infect other types of cells colonising this new area.
- By infecting WBCs they cause them to send out faulty messages. These are called cytokines, proteins that regulate inflammatory responses in the body.
In the American Society for Microbiology, it noted
“… we propose to regard the attenuated release capacity of white blood cells for proinflammatory cytokines such as TNF-α and IFN-γ as a mechanism that weakens the immune response of borreliosis patients to circulating spirochetes.” Isabel Diterich, et al (2001)
Use of antibiotics during the active acute (or initial) phase of Lyme disease will often reduce the concentration of Borrelia. With reduced numbers to deal with the immune system has a better chance to clear the microbes before they get established in tissues. The problem is that antibiotics alone do not eliminate the tick-borne disease as noted below.
“Using multiple corroborative detection methods, we showed that patients with persistent Lyme disease symptoms may have ongoing spirochetal infection despite antibiotic treatment, similar to findings in non-human primates.” M. J. Middelveen et al (2018)
“It is known that Lyme borreliosis mimics multiple diseases that were never proven to have a spirochaete aetiology. Using complete modified Kelly-Pettenkofer medium we succeeded in cultivating live B. burgdorferi sensu lato spirochaetes from samples taken from people who suffered from undefined disorders, had symptoms not typical for Lyme borreliosis, but who had undergone antibiotic treatment due to a suspicion of having Lyme disease even though they were seronegative. We report the first recovery of live B. burgdorferi sensu stricto from residents of southeastern USA and the first successful cultivation of live Borrelia bissettii-like strain from residents of North America. Our results support the fact that B. bissettii is responsible for human Lyme borreliosis worldwide along with B. burgdorferi.” Rudenko N. et al (2016)
It would seem in fact it is difficult to treat with antibiotics when the infection is chronic. What does this mean? Basically, this means it’s up to your immune system to contain or eradicate the microbe.
For your immune system to function at optimal levels the white blood cells must communicate with one another and every other cell in your body. This is so the immune system can synchronize their efforts successfully.
What does borrelia do? It specializes in disrupting cell-to-cell communication and it doesn’t take many infected WBCs to cause a disturbance which then allows Borrelia microbes to become established in tissues. In other words, the borrelia becomes invisible to your immune system.
There is light at the end of the tunnel though.
Certain herbals work against not only borrelia but also coinfections. Why? Because they have a defence system which protects the plant by killing pathogens. We can harness that ability to our own advantage when dealing with Lyme and Lyme-like issues.
Resources
Isabel Diterich, et al, (2001) Modulation of Cytokine Release in Ex Vivo-Stimulated Blood from Borreliosis Patients. Infect Immun. 2001 Feb; 69(2): 687–694. doi: 10.1128/IAI.69.2.687-694.2001
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC97940/
M.J. Middelveen, et al. (2018) Persistent Borrelia Infection in Patients with Ongoing Symptoms of Lyme Disease. Published online 2018 Apr 14. doi: 10.3390/healthcare6020033. https//www.ncbi.nlm.nih.gov/pmc/articles/PMC6023324/
